 Structural Racism and Anti-Blackness in Medicine
Structural Racism and Anti-Blackness in Medicine
are Unacceptable and Must Be Addressed
Recent events in the US have included protests against the brutality meted out to Black Americans by the criminal justice system, and exposure of the disparate impact of the COVID-19 pandemic on communities of color engendered by social and economic inequality, with its consequences for housing and health care. These events have sparked a long-overdue societal examination of the impact of structural racism. Certainly, the Wang N article, entitled “Diversity, Inclusion, and Equity: Evolution of Race and Ethnicity…” published March 2020 in JAHA is horribly incorrect, harmful, and promotes racial discrimination. In the process, issues of “white privilege” and implicit bias cry out for attention by all citizens, and the hope for redress has again been enkindled. Medical education and postgraduate training are areas in special need.
In this spirit, the Association of Black Cardiologists issues a call to our professional colleagues to participate with us in activities and approaches that seek to enhance awareness of structural problems and to embark on specific corrective strategies. Though medical education and postgraduate training have their own special needs, the ultimate goal is to improve the health status – cardiovascular and total – of Black Americans and other disadvantaged minorities by actions that improve access to and use of high-quality health care.
General approaches include:
- Continued and concerted efforts to remove roadblocks to the preparation for and training of minority students for careers in health care.
- Specific training on sensitivity to issues of white privilege and implicit bias at all levels of medical training and administration.
- Professional support for social and legislative measures to ensure universal health care.
- Increased advocacy for research and publication of data on health disparities, including issues of minority patient and main principal investigator representation in clinical trials, and minority involvement in editorial processes.
- Recognition that the “minority tax” can become a toxic experience that affects health and should be given appropriate consideration in promotion and advancement in all spheres of medicine.
Strategies related to research and publications should include:
- Increasing diversity in research-related activities (e.g clinical trial diversity of patients, main principal investigators who are Black or Hispanic/LatinX)
- Ensuring racial, ethnic and gender diversity on editorial boards including for editors; groom diverse persons to assume these positions.
- Assigning equal value to racial and ethnic related disparities research as given to other types of research by journals and funding entities.
- Requiring that the review of articles pertaining to racial and ethnic diversity and related topics involve scholars in these areas.
Affiliated Resources
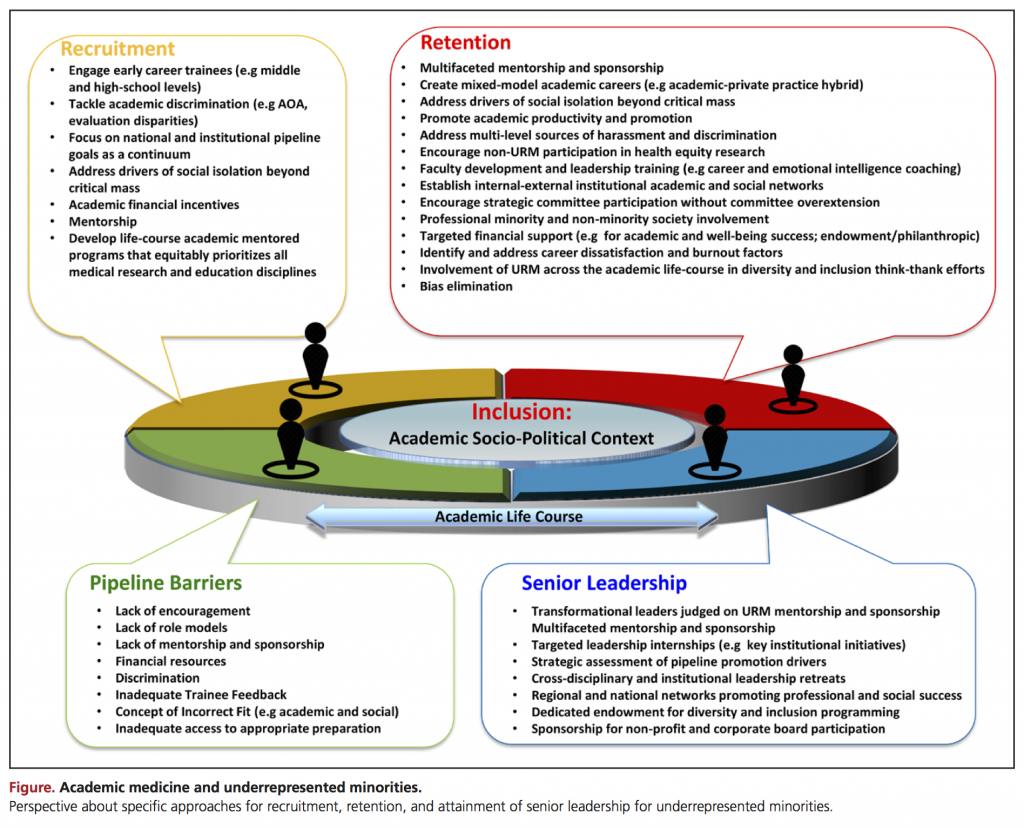
#Me_Who: Anatomy of Scholastic, Leadership, and Social Isolation of Underrepresented Minority Women in Academic Medicine
Dr. Michelle A. Albert, Circulation, May 22, 2018, Volume 137, Issue 21
Joint Statement on Health Equity, Social Justice, and Civil Unrest
From the Association of Black Cardiologists, American Heart Association and American College of Cardiology, May 30, 2020
Blacks in Medicine: Clinical, Demographic, and Socioeconomic Correlations
Dr. Richard Allen Williams, Springer International Publishing, June 2020
